- Summary
- Symptoms
- Read More
Summary
Hallux limitus describes a condition where the hallux (great toe) is limited in its range of motion at the metatarsal phalangeal joint. This limited range of motion results in pain of the 1st metatarsal phalangeal joint (1st mpj or great toe joint.) If left untreated, hallux limitus will progress to arthritis of the great toe joint. The most characteristic sign of hallux limitus is a bump (exostosis) on top of the head of the 1st metatarsal. Based on this clinical finding, many doctors also refer to hallux limitus as a dorsal bunion. Hallux limitus is found equally in men and women. The onset of hallux limitus is between the ages of 20 and 50 years.
Symptoms
- Limited range of motion of the great toe joint
- Pain with range of motion of the great toe joint
- Dorsal exostosis often referred to as a dorsal bunion
Description
 Hallux limitus is caused by four contributing factors. These factors include the following:
Hallux limitus is caused by four contributing factors. These factors include the following:
1. A long 1st metatarsal.
2. An elevated 1st metatarsal (metatarsus primus elevatus.)
3. An impaction injury of the 1st mpj resulting in an osteochondral defect (OCD) of the joint.
4. Systemic diseases that cause injury to the joint, such as rheumatoid arthritis, lupus or gout.
Hallux limitus is graded in four stages:
| Symptoms | External appearance of the joint | X-ray findings | Treatment | |
| Stage 1 | Vague joint pain | No change evident | No changes noted | Dancer's pad or sub 1 cut out in an orthotic. |
| Stage 2 | Increased frequency and duration of pain | Mild dorsal exostosis | Dorsal exostosis on lateral x-ray | Carbon plate with Morton's extension (turf toe plate or Spring Plate.) Possible joint revision. |
| Stage 3 | Pain with all activities | Large dorsal exostosis | Increased dorsal exostosis. Asymmetrical joint space narrowing | Turf toe plate or Spring Plate. Cheilectomy or Youngswick osteotomy with joint revision. |
| Stage 4 | Significant pain with any range of motion of the joint | Enlargement of the entire joint | Flattening of the joint with prolific spurring surrounding the entire joint | Joint replacement, fusion or Keller bunionectomy |
Causes and contributing factors
 Most cases of hallux limitus are due to a long 1st metatarsal that results in metatarsus primus elevatus. Normal function of the great toe joint (1st metatarsal phalangeal joint) requires that the 1st metatarsal bone plantarflex (move down) to allow the proximal phalanx to ride up (dorsiflex.) This hinge action needs to take place with each step. If the normal range of motion is limited in any way, jamming of the joint will occur and hallux limitus will ensue.
Most cases of hallux limitus are due to a long 1st metatarsal that results in metatarsus primus elevatus. Normal function of the great toe joint (1st metatarsal phalangeal joint) requires that the 1st metatarsal bone plantarflex (move down) to allow the proximal phalanx to ride up (dorsiflex.) This hinge action needs to take place with each step. If the normal range of motion is limited in any way, jamming of the joint will occur and hallux limitus will ensue.
There are two known biomechanical factors that contribute to the formation of hallux limitus. Those factors include:
A long 1st metatarsal - the relative length of the 1st and second metatarsals is very important in understanding the onset of hallux limitus. To explain the relevance of a long 1st metatarsal, consider this example: you have two bamboo poles that you hold under your left and right arms and extend directly out in front of you. The pole on the left is 5 feet long and the pole on the right is 10 feet long. You slowly lower the poles to the ground and the long (right) pole will hit the ground first, followed by the shorter pole hitting the floor last. Now imagine the two poles as the 1st and 2nd metatarsals of the left foot or right foot. For effective function of the great toe joint, the 1st metatarsal has to be that shorter pole. If it is longer, the normal hinge action will not occur and jamming will ensue.
An elevated 1st metatarsal (metatarsus primus elevatus) - as previously described, plantarflexion of the 1st metatarsal is required for the hallux to ride up onto the 1st metatarsal head. With an elevated 1st metatarsal, the hinge motion is limited and jamming ensues.
Differential diagnosis
The differential diagnosis for hallux limitus includes:
Arthritis
Bunion
Gout
Pseudogout
Septic joint
Sesamoiditis
Sesamoid fracture
Treatment
 The diagnosis and treatment of hallux limitus begins with the evaluation of the range of motion of the great toe joint. Evaluation of the range of motion of the 1st mpj can be performed in two positions: relaxed and functional. In a relaxed position, with no resistance exerted by the calf, the 1st mpj shows normal range of motion without pain. In a functional position, when resistance is applied by the calf, the range of motion of the 1st mpj changes and hallux limitus can be more appropriately assessed. The term functional hallux limitus is applied to cases that have normal range of motion in a relaxed position but decreased range of motion in a functional position.
The diagnosis and treatment of hallux limitus begins with the evaluation of the range of motion of the great toe joint. Evaluation of the range of motion of the 1st mpj can be performed in two positions: relaxed and functional. In a relaxed position, with no resistance exerted by the calf, the 1st mpj shows normal range of motion without pain. In a functional position, when resistance is applied by the calf, the range of motion of the 1st mpj changes and hallux limitus can be more appropriately assessed. The term functional hallux limitus is applied to cases that have normal range of motion in a relaxed position but decreased range of motion in a functional position.
Assessment of hallux limitus requires evaluation of the 1st mpj in both a relaxed and functional position. Is there crepitus (grating or cracking) with range of motion? Does the joint catch or pop? Is there pain with range of motion? Each of these signs indicate different stages of hallux limitus.
Conservative care of stage 1 hallux limitus may include the use of a dancer's pad or orthotic custom made with a sub 1 cut out pad. These two types of pads are used in an attempt to increase the plantarflexion of the 1st metatarsal to improve range of motion of the 1st mpj. As we progress into more advanced stages of hallux limitus (2-4), the dancer's pads will no longer be effective. In stage 2 we change treatment to a stiff carbon graphite insert with a rigid extension called a Morton's extension. A Morton's extension is used to stiffen the shoe to decrease painful range of motion. Another short-term solution for stage 2-4 is to use a turf toe strap to limit range of motion.
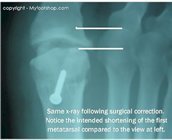
Injectable cortisone is often used to treat hallux limitus. There is some debate as to the merit of using cortisone to treat hallux limitus. As noted above, the majority of cases of hallux limitus are due to aberrations in the biomechanical properties of the 1st mpj. Therefore, common sense would say that the most effective method of treatment for hallux limitus would be to change or alter the biomechanical property that is causing the problem. For instance, if hallux limitus is due to a long first metatarsal, then the optimal treatment would be to shorten the first metatarsal. Cortisone cannot treat these biomechanical factors and therefore must have only a minimal role in the treatment of hallux limitus.
There are a number of surgical procedures used to correct hallux limitus. One method of care is a procedure called a cheilectomy. Cheil is French for lip and a cheilectomy is a procedure that focuses exclusively on resection of the dorsal exostosis (the lip) of the 1st metatarsal head. A second type of surgery for hallux limitus is a metatarsal osteotomy and cheilectomy. The metatarsal osteotomy, often called a Youngswick's modification of an Austin bunionectomy, creates a break in the bone that can either shorten or plantarflex the head of the metatarsal. The osteotomy is important because it addresses the primary reason for hallux limitus (metarsus primus elevatus and a long first metatarsal.) It should be noted that there is not universal agreement among doctors as to which of these procedures is the best solution for hallux limitus.
procedure called a cheilectomy. Cheil is French for lip and a cheilectomy is a procedure that focuses exclusively on resection of the dorsal exostosis (the lip) of the 1st metatarsal head. A second type of surgery for hallux limitus is a metatarsal osteotomy and cheilectomy. The metatarsal osteotomy, often called a Youngswick's modification of an Austin bunionectomy, creates a break in the bone that can either shorten or plantarflex the head of the metatarsal. The osteotomy is important because it addresses the primary reason for hallux limitus (metarsus primus elevatus and a long first metatarsal.) It should be noted that there is not universal agreement among doctors as to which of these procedures is the best solution for hallux limitus.
 Many surgeons believe that hallux limitus can be corrected with a simple cheilectomy. The advantage to performing just a cheilectomy is that a person will regain some range of motion and be back on their feet relatively quickly. The disadvantage to performing just the cheilectomy without osteotomy is that the primary biomechanical reason for hallux limitus will not be addressed. In time, the dorsal lip will return and arthritis within the joint will increase. The disadvantage of an osteotomy is that it increases the difficulty of the surgery and increases healing time.
Many surgeons believe that hallux limitus can be corrected with a simple cheilectomy. The advantage to performing just a cheilectomy is that a person will regain some range of motion and be back on their feet relatively quickly. The disadvantage to performing just the cheilectomy without osteotomy is that the primary biomechanical reason for hallux limitus will not be addressed. In time, the dorsal lip will return and arthritis within the joint will increase. The disadvantage of an osteotomy is that it increases the difficulty of the surgery and increases healing time.
Cheilectomy and osteotomies are procedures applicable to stage 2 and 3 hallux limitus. In addition to these procedures, revision of the joint may be performed to repair or induce regeneration of the cartilage. Transchondral drilling is a technique used to resurface the joint during surgery. Transchondral drilling means that a fine drill is used to drill through the hard layer of bone (subchondral bone) just beneath the surface of the cartilage. Drilling provides access to bone cells in the marrow of the bone that may become cartilage cells. These cells are known as pleuri-potential cells and are considered a form of stem cell. Another technique used to resurface the joint involves the use of an osteochondral graft often referred to as an OAT procedure or osteo-articular transfer. OAT grafts can be harvested from other joints (often the knee) to transfer to the damaged cartilage of the 1st mpj. Synthetic bone graft material and metallic implants can also be used for joint resurfacing.
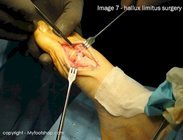
The following images show the surgical steps used to correct stage 3 hallux limitus. This procedure is called the Youngswick modification of an Austin bunionectomy. Image 1 shows the pre-operative planning with incision line and joint space marked. Image 2 shows exposure of the dorsal exostosis (also called a dorsal bump or dorsal bunion.) In Image 3, we see an oscillating saw resecting the dorsal exostosis. This procedure is called a cheilectomy. Image 4 shows erosion of the cartilage of the head of the 1st metatarsal (stage 3 chondromalacia.) A 1.2 mm pin of Kirschner wire is being used to perform subchondral drilling. Subchondral drilling can help to restore damaged cartilage. Image 5 shows the osteotomy of the 1st metatarsal. A 2 mm wedge is being taken from the dorsal aspect of the osteotomy. The osteotomy is outlined by blue dots. Image 6 shows the completed osteotomy that has shortened and plantarflexed the 1st metatarsal. Image seven shows fixation of the osteotomy with a single screw. Image 8 shows the improved range of motion post-op. In Image 9, the joint capsule and deep tissue are closed. Image 10 shows final skin closure.
Surgical correction of hallux limitus is performed at a hospital or outpatient center. The procedure takes approximately 1 hour to complete. A local anesthetic with sedation or general anesthesia is used. Patients are able to bear weight on the foot immediately post-op for limited periods of time. A walking cast will be used for 6 weeks post-op. Variations in this procedure may include K wire fixation or absorbable pin fixation. The long-term success of this procedure is good if performed on stage two and early stage three patients.
Conservative care of hallux rigidus (stage 4 hallux limitus) focuses on the use of pads to limit the range of motion of the great toe or devices to stiffen the shoe. Turf toe straps are a great short-term aid for symptoms of hallux limitus and hallux rigidus. Turf toe plates and carbon spring plates are two examples of inserts that can be used to stiffen the shoe. Shoe modifications are also used to decrease bending of the forefoot. The most common modification is called an anterior rocker sole, seen at right.
stiffen the shoe. Turf toe straps are a great short-term aid for symptoms of hallux limitus and hallux rigidus. Turf toe plates and carbon spring plates are two examples of inserts that can be used to stiffen the shoe. Shoe modifications are also used to decrease bending of the forefoot. The most common modification is called an anterior rocker sole, seen at right.
 Surgical repair of stage 4 hallux limitus (hallux rigidus) again has disagreement among doctors as to the best choice of procedure. In stage 4, often referred to as hallux rigidus, the surface of the joint is so badly damaged that the joint is not salvageable. Implant arthroplasty is one choice. Implant arthroplasty involves resection of the joint and replacement of the joint with an implant. The advantage of implant arthroplasty is that the implant will maintain the normal length of the toe and preserve normal range of motion. Another technique used in stage 4 hallux limitus is fusion of the 1st mpj. Fusion of the joint requires a period of non-weight bearing for proper healing. The disadvantage of 1st mpj healing is that the toe may be shortened due to resection of the joint. A bone graft may be taken from the hip to supplement length. Another disadvantage of fusion is permanent stiffness of the 1st mpj. The last option for stage 4 hallux limitus is a Keller bunionectomy. A Keller bunionectomy is a procedure where the base of the great toe is resected and a new joint created using a flap of the joint capsule. This technique is called an interpositional arthroplasty - interposing the soft tissue to create a joint. The advantage of a Keller bunionectomy is that it is easy for patients to get back on their feet. The disadvantage is that the great toe becomes loose, short and floppy.
Surgical repair of stage 4 hallux limitus (hallux rigidus) again has disagreement among doctors as to the best choice of procedure. In stage 4, often referred to as hallux rigidus, the surface of the joint is so badly damaged that the joint is not salvageable. Implant arthroplasty is one choice. Implant arthroplasty involves resection of the joint and replacement of the joint with an implant. The advantage of implant arthroplasty is that the implant will maintain the normal length of the toe and preserve normal range of motion. Another technique used in stage 4 hallux limitus is fusion of the 1st mpj. Fusion of the joint requires a period of non-weight bearing for proper healing. The disadvantage of 1st mpj healing is that the toe may be shortened due to resection of the joint. A bone graft may be taken from the hip to supplement length. Another disadvantage of fusion is permanent stiffness of the 1st mpj. The last option for stage 4 hallux limitus is a Keller bunionectomy. A Keller bunionectomy is a procedure where the base of the great toe is resected and a new joint created using a flap of the joint capsule. This technique is called an interpositional arthroplasty - interposing the soft tissue to create a joint. The advantage of a Keller bunionectomy is that it is easy for patients to get back on their feet. The disadvantage is that the great toe becomes loose, short and floppy.
Implant arthroplasty (joint replacement) involves resection of the joint and replacement of the joint with a flexible hinge. The following images show the steps used to perform implant arthroplasty of the great toe joint. Image 1 shows the pre-op planning and location of the incision. Images 2 and 3 show dissection of the joint and removal of arthritic spurring surrounding the joint. Image 4 shows the trial implant sizers. Images 5-8 show remodeling of the joint with preparation of the implant site. Images 9-12 show placement of the implant and final closure. This procedure is performed at a hospital or surgery center under general anesthesia or local anesthesia with sedation. The procedure takes about an hour to complete. Patients can bear full weight on the foot immediately following surgery.
When to contact your doctor
Pain and limitation of the range of motion of the great toe should be evaluated by your podiatrist or orthopedist to rule out hallux limitus.
References
References are pending.
Author(s) and date
![]() This article was written by Myfootshop.com medical advisor Jeffrey A. Oster, DPM.
This article was written by Myfootshop.com medical advisor Jeffrey A. Oster, DPM.
Competing Interests - None
Cite this article as: Oster, Jeffrey. Hallux Limitus. https://www.myfootshop.com/article/hallux-limitus
Article most recently updated: December 10, 2020.
 Hallux Limitus by Myfootshop.com is licensed under a Creative Commons Attribution-NonCommercial 3.0 Unported License.
Hallux Limitus by Myfootshop.com is licensed under a Creative Commons Attribution-NonCommercial 3.0 Unported License.
Internal reference only: ZoneP5, ZoneD7, ZoneL11, ZoneM9