History of Lisfranc injuries
Jaques Lisfranc de St. Martin was a French physician, pioneering many surgical procedures during the early 19th century. As a surgeon in the Napoleonic army, Lisfranc worked on the Russian front where he acquired acclaim for his skill in working with foot injuries. It is said that Lisfranc studied French soldiers who fell from horses while their foot was still in the stirrup. The resulting injury was a unique fracture/dislocation of the midfoot. This series of joints and their pattern of injuries is now called Lisfranc’s joint, Lisfranc’s dislocation and Lisfranc’s fracture.
Treatment of Lisfranc injuries
Lisfranc injuries (fracture, dislocation and combined fracture/dislocation) are complex injuries that can have life long disability for patients. Reduction and repair of these injuries begins with a high degree of clinical suspicion at the time ofinjury and upon presentation to the ED. The envelope of soft tissue (joint capsule, ligament, tendons and skin) surrounding the midfoot is often strong enough to contain the injury resulting in difficulty seeing the complex and often multiple fractures of the midfoot. Numerous classification schemes (Quenu and Kuss, Hardcastle and Myerson) have been well described in the literature and guide conservative and surgical treatment options.
Post-operative care of Lisfranc injuries
What Lisfranc failed to provide us though is a guide or manual for patients and surgeons to coordinate post-operative care. Anatomical reduction in surgery is imperative, but how do we manage post operative care of these complex injuries?
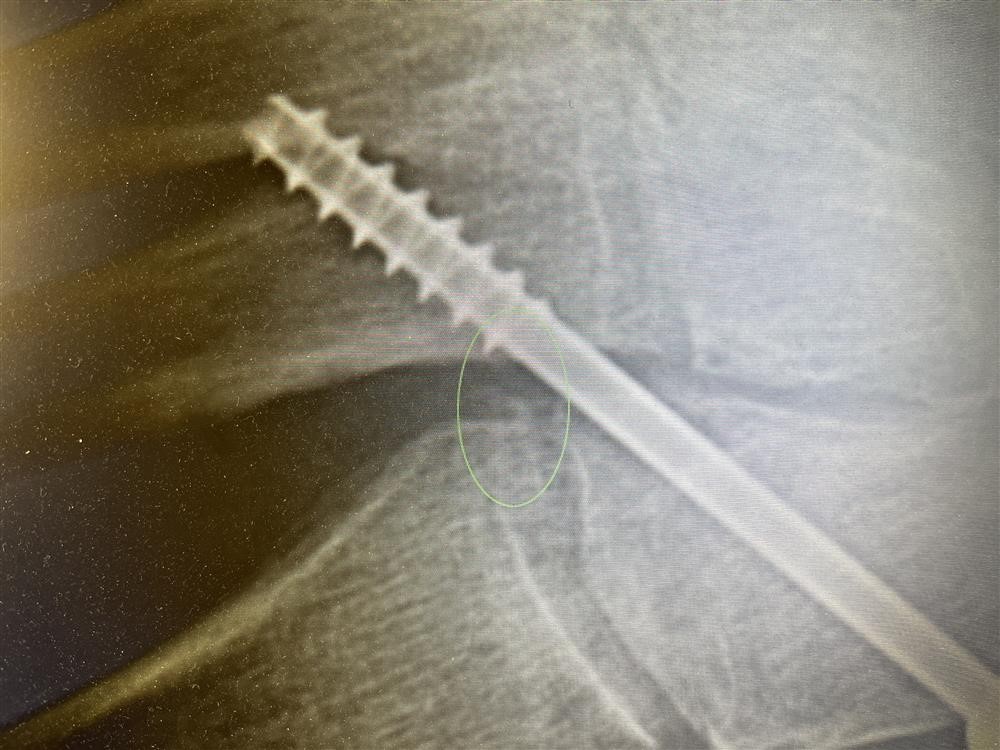
The image at left shows a repair of a Lisfranc dislocation and associated fractures of metatarsals 2/3. Highlighted is the fleck sign, a small fleck of bone associated with an avulsion of bone by Lisfranc ligament.
The screw seen in this image is temporary fixation. With prolonged weight bearing, the screw will break and become almost impossible to retrieve.
Each Lisfranc injury is unique and requires individualized care. In most cased, after reduction and percutaneous fixation, I return patients to early, non-weight bearing range of motion at 4 weeks. Weight bearing may begin at 8 weeks. Knowing that patients will begin weight bearing with crutches and tentative load bearing, I allow my patient to bear weight for 3-4 weeks. By doing so, I utilize the internal fixation for a full 10 to 12 weeks. Removal of the fixation is an outpatient procedure.
Return to weight bearing - the use of carbon fiber spring plates
Return to weigh bearing post Lisfranc injury can also be facilitated by use of a rigid shoe and the use of 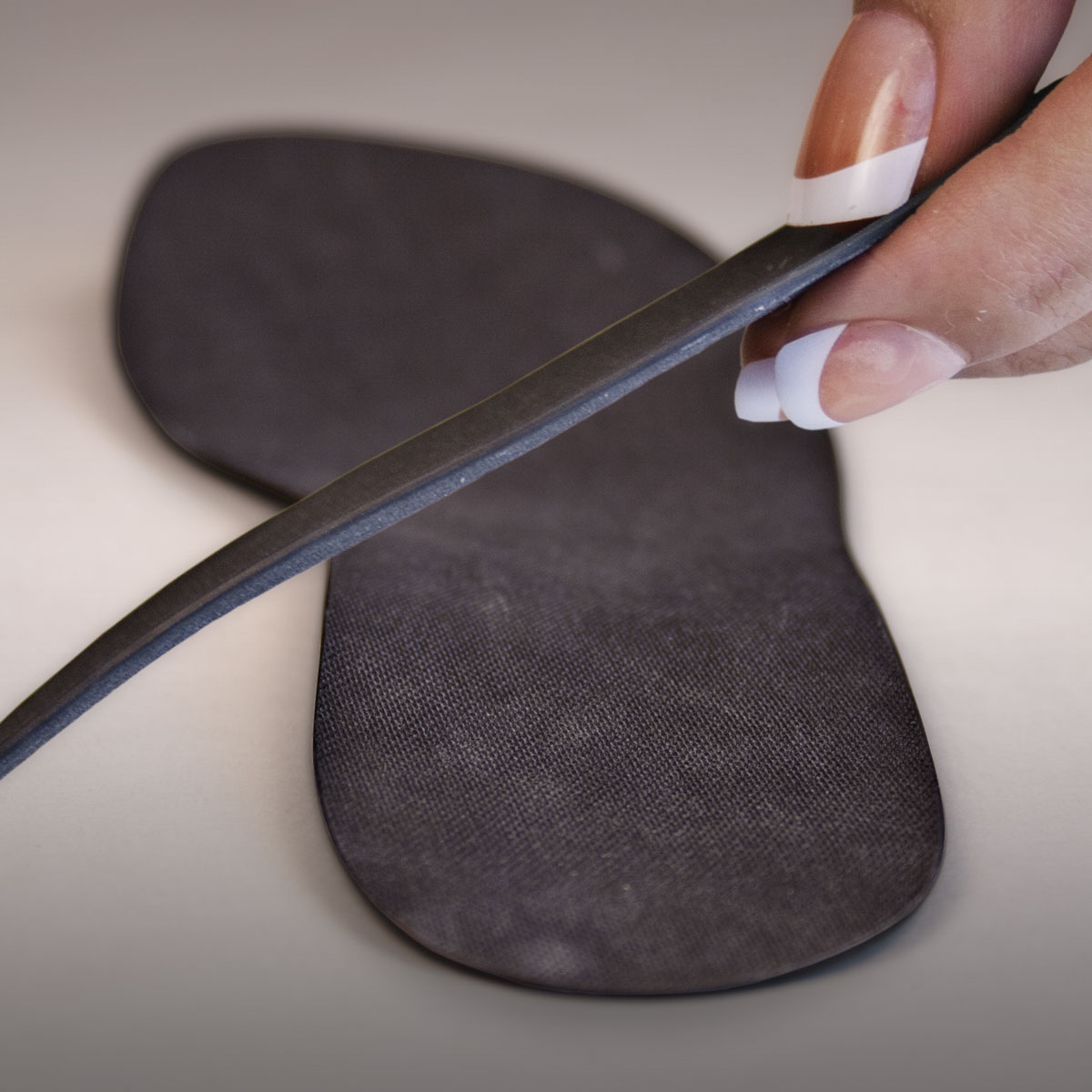 a carbon fiber spring plate. In a laced shoe, a rigid shoe shank helps to act as a brace for the midfoot. Similarly, a carbon fiber insole also helps to support the midfoot, stabilizing the Lisfranc injury.
a carbon fiber spring plate. In a laced shoe, a rigid shoe shank helps to act as a brace for the midfoot. Similarly, a carbon fiber insole also helps to support the midfoot, stabilizing the Lisfranc injury.
Return to activities post Lisfranc injury can be prolonged and are best staged, starting with brief periods of weight bearing and increasingly longer periods of weight bearing based on pain and swelling. Physical therapy can be very helpful in return to weight bearing, helping guide the patient in making choices regarding activities and duration of weight bearing.
Jeff
Medical Advisor
Myfootshop.com