- Summary
- Osteo
- Rheumatoid
- Psoriatic
- Reiter's Syndrome
- Read More...
Summary
Arthritis is an inflammatory condition of one or more joints. There are many different types of arthritis. Each type of arthritis has a characteristic group of symptoms such as onset, location, and type of pain. Arthritis may be called mono-articular or polyarticular depending upon the number of joints involved. If left untreated, arthritis may result in progressive erosion of the surface cartilage and instability of the joint. This article discusses the four most common types of arthritis commonly found in the foot and ankle: osteoarthritis, rheumatoid arthritis, psoriatic arthritis, and Reiter's Syndrome. Gout and pseudogout are crystal deposition diseases that may cause arthritis. These two conditions are discussed in separate articles.
Symptoms
The onset, severity, and duration of symptoms vary with each type of arthritis. Please refer to each arthritis type described in this article.Osteoarthritis
Osteoarthritis (OA) is by far the most common form of arthritis found in the foot and ankle and will affect most of us over the course of our lives. Osteoarthritis increases with age and is often the result of previous or repetitive injury to the joint. Additional contributing factors to osteoarthritis include genetic predisposition to osteoarthritis. The classifications used to describe osteoarthritis include primary (idiopathic or no known cause) and secondary (some known cause for the disease such as trauma.)
Osteoarthritis is a complex disease that is the result of several different processes that take place simultaneously both within and peripheral to the joint. The onset of osteoarthritis begins with a series of small micro-fractures that occur in the bone immediately adjacent to the joint called subchondral bone. In a young, healthy individual, subchondral bone acts as a shock absorber for loads applied to the joint. With progressive age, subchondral bone becomes brittle and susceptible to injury. As load is applied to the subchondral bone, it breaks, resulting in micro-fractures. The more the joint is used the more the subchondral bone breaks down. The repetitive breakdown and repair of the bone results in enlargement (hypertrophy) of the joint margins. The appearance of osteoarthritis in the hands is the enlargement of the joints of the fingers, classically called Heberden's Nodes.
occur in the bone immediately adjacent to the joint called subchondral bone. In a young, healthy individual, subchondral bone acts as a shock absorber for loads applied to the joint. With progressive age, subchondral bone becomes brittle and susceptible to injury. As load is applied to the subchondral bone, it breaks, resulting in micro-fractures. The more the joint is used the more the subchondral bone breaks down. The repetitive breakdown and repair of the bone results in enlargement (hypertrophy) of the joint margins. The appearance of osteoarthritis in the hands is the enlargement of the joints of the fingers, classically called Heberden's Nodes.
As the micro-fractures in subchondral bone progress, the ability of the subchondral bone to support the joint surface and cartilage becomes compromised. As a result, when the joint attempts its normal range of motion, the cartilage is irregular and progressively erodes. The irregular surface of the cartilage may result in loss of range of motion and pain. Cartilage has no nerve endings to sense pain, but the subchondral bone is filled with nerve endings. As the cartilage is eroded, subchondral bone becomes exposed, resulting in significant pain with bone-on-bone contact within the joint. Peripheral spurring of the joint is also another contributing factor to pain that is very common in osteoarthritis. Peripheral spurring will also limit the normal range of motion of the joint.
The tissue surrounding a joint may also contribute to osteoarthritis. Joints are surrounded by a joint capsule that encompasses the entire joint. The joint capsule is lined with tissue called synovium. Synovium produces the fluid or lubricant that makes the joint slippery. In cases of osteoarthritis, the quantity and the quality of the synovial fluid changes and becomes a less desirable lubricant for the joint. Change in synovial fluid will affect the health of the joint in several ways. Cartilage cells, known as chondrocytes, are avascular and derive all of their oxygen and nutrition from the synovial fluid. Therefore, changes in the synovial fluid will have a direct impact on the viability of the cartilage. Change in the synovial fluid will also limit the range of motion of the joint.
A normal, healthy joint will have a very tight external envelope consisting of ligaments, tendons, and joint capsules. As osteoarthritis progresses, this envelope will become slack and contribute to instability of the joint. Joint instability will, in turn, result in additional physical damage to the joint.
A history of injury to a joint will affect how quickly the joint deteriorates. Injury to the joint may directly affect the cartilage, subchondral bone or surrounding capsule that holds the joint intact. We all know someone with an old football injury of the knee who develops osteoarthritis early in their adult life. Joint erosion seems to occur at different rates in different individuals. In fact, every joint in the body seems to undergo the changes of osetoarthritis at different rates.
Symptoms
The onset and symptoms of osteoarthritis in the foot and ankle can vary dramatically based on foot type, previous injury, and genetic predisposition to osteoarthritis. The most common location of osteoarthritis in the foot is in the midfoot or arch. The midfoot is a complex configuration of bones that are held together by thick, inelastic ligaments. Symptoms of osteoarthritis of the midfoot include pain and stiffness with the onset of activity such as getting out of bed in the morning or standing after a brief period of rest. Firm swelling through the midfoot is a common complaint. Additional symptoms include the inability to wear unsupportive shoes such as flip-flops or sandals.
the midfoot or arch. The midfoot is a complex configuration of bones that are held together by thick, inelastic ligaments. Symptoms of osteoarthritis of the midfoot include pain and stiffness with the onset of activity such as getting out of bed in the morning or standing after a brief period of rest. Firm swelling through the midfoot is a common complaint. Additional symptoms include the inability to wear unsupportive shoes such as flip-flops or sandals.
Forefoot osteoarthritis is also common and may be joint specific. Isolated osteoarthritis of the great toe joint is called hallux limitus or hallux rigidus. Symptoms of hallux limitus include stiffness and pain with range of motion.
Osteoarthritis of the rearfoot and ankle is often a result of previous injury such as prior ankle fracture or repetitive ankle sprains. Symptoms of rearfoot and ankle arthritis include stiffness and pain with weight bearing.
Causes and Contributing Factors
The underlying cause of OA is unknown, but it seems to have both a genetic predisposition and relationship to joint trauma. Many authors speculate that the cause may be mechanical, as discussed above, but others describe changes such as biologic, biochemical, enzymatic or even a combination of these.
Treatment
Osteoarthritis, regardless of the location, is treated with bracing, anti-inflammatory medications, and surgery. Treatment begins with shoes and braces to make the foot more efficient. The less work the foot performs, the more we can control the symptoms of osteoarthritis. Treatment may include:
-
Oxford shoes with a rigid shank and stiff-laced uppers
-
Carbon plates to stiffen the shank or stiffen the forefoot
-
Bracing with an Arizona Brace or Ritchie Brace
Oral or topical anti-inflammatories can help in the acute phase of osteoarthritis. Non-steroidal anti-inflammatories (NSAIDs) often are used. Examples of NSAID's include Celebrex, Naprosyn, and Motrin. Topical pain relievers such as Biofreeze also are helpful.
Injectable hylan G-F 20 (Synvisc), or what is called viscosupplementation, is popular for large joints including the ankle. Although this is still considered an "off-label" use of Synvisc, studies show an injection can reduce the symptoms of osteoarthritis for 3 to 12 months. Synvisc often is used in conjunction with arthroscopic debridement of the ankle.
 Surgical treatment of osteoarthritis may be required if bracing and medical treatment proves ineffective. Surgical care consists of joint debridement, fusion or replacement with implants. The choice of each procedure depends on the location of the osteoarthritis and general health of the patient.
Surgical treatment of osteoarthritis may be required if bracing and medical treatment proves ineffective. Surgical care consists of joint debridement, fusion or replacement with implants. The choice of each procedure depends on the location of the osteoarthritis and general health of the patient.
For end-stage rearfoot and ankle osteoarthritis, joint fusion has been a trusted and reliable procedure used for many years. Fusion procedures are performed at a hospital under general anesthesia, taking from 1 to 2 hours to complete. The joint that is undergoing fusion is resected (removed) and the joint is fixated by internal or external fixation. The fusion site remains stabilized for 10-12 weeks following surgery to ensure bony fusion. For most patients who undergo subtalar joint or ankle fusion, gait is normal at slow speeds (walking) but limits any activity, such as running.
 Correction of ankle arthritis using ankle implant surgery has become common in the past few years. Several unique styles of implant have been approved by the FDA for ankle replacement. Ankle replacement surgery is a new field that has shown promising early results. Unfortunately, the long-term success of ankle implants has been less than optimal for most patients. Revision of failed ankle implants is difficult due to the amount of bone resected to place the implant. Mechanical failure continues to be common in ankle implants. Ankle fusion remains a common alternative to ankle implants. Ankle implant surgery is performed under general anesthesia and takes 1-2 hours to complete. The ankle is then immobilized for 4 weeks following surgery, at which time patients can begin to bear weight on the ankle.
Correction of ankle arthritis using ankle implant surgery has become common in the past few years. Several unique styles of implant have been approved by the FDA for ankle replacement. Ankle replacement surgery is a new field that has shown promising early results. Unfortunately, the long-term success of ankle implants has been less than optimal for most patients. Revision of failed ankle implants is difficult due to the amount of bone resected to place the implant. Mechanical failure continues to be common in ankle implants. Ankle fusion remains a common alternative to ankle implants. Ankle implant surgery is performed under general anesthesia and takes 1-2 hours to complete. The ankle is then immobilized for 4 weeks following surgery, at which time patients can begin to bear weight on the ankle.
Another technique called arthrodiastasis involves off-loading the ankle with a distraction fixator. The fixator is surgically attached to the foot and leg with pins. The pins then are mechanically separated to "off-load" the ankle. The theory is that off-loading allows the joint to regenerate cartilage. Arthrodiastasis requires 12 to 22 weeks of non-weight-bearing in the distractor.
Rheumatoid Arthritis
Rheumatoid arthritis (RA) is a complex and debilitating disease that affects about 1 percent of the general population. Rheumatoid arthritis is an autoimmune disease that affects women three times more than men. Rheumatoid arthritis can be subcategorized as seropositive or seronegative. The vast majority of rheumatoid arthritis is seropositive, meaning that the patient's blood sample will react in the lab with the autoantibody that causes rheumatoid arthritis. Symmetrical involvement is typical, with both hands and both feet affected. In comparison to osteoarthritis (OA), morning stiffness associated with RA will last more than 30 minutes.
Symptoms
Symptoms of rheumatoid arthritis include an acute onset of pain accompanied by joint swelling. The onset of pain is polyarticular and limits most activities, including the ability to work. The onset of rheumatoid arthritis in the foot is abrupt, usually within a matter of hours. Rheumatoid arthritis often progresses to subluxation of the metatarsal phalangeal joints. Rheumatoid nodules and atrophy of the plantar fat pad are common.
Causes and Contributing Factors
RA is an autoimmune disease. An autoimmune disease occurs when the body's immune system attacks itself. In the case of RA, the immune system attacks the cells lining the joint capsule called the synovium. The end result is thickening and fibrosis of the joint with destruction of the cartilage.
Treatment
 Treatment of rheumatoid arthritis in the foot can be quite complex and depends on the patient's response to treatment. Medical care of rheumatoid arthritis should be managed by a rheumatologist who is familiar with the side effects of medications that reduce the body's autoimmune response.
Treatment of rheumatoid arthritis in the foot can be quite complex and depends on the patient's response to treatment. Medical care of rheumatoid arthritis should be managed by a rheumatologist who is familiar with the side effects of medications that reduce the body's autoimmune response.
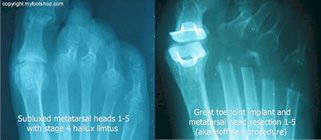
Although treatment of the immune response is the primary goal in RA, bracing and joint support are critical. Surgical revision of joints affected by RA is common. The image at left shows the pre and post-surgical correction of rheumatoid deformity of the forefoot. The pre-op image at left shows dislocation of the metatarsal phalangeal joints and advanced rheumatoid arthritis of the great toe joint. The adjacent post-op image shows a Swanson great toe implant and pan-metatarsal head resection (Hoffman Procedure.)
Psoriatic Arthritis
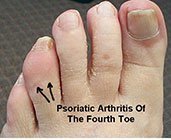
Psoriatic arthritis (PA) is form of sero-negative arthritis. Psoriatic arthritis may be associated with a previous skin or nail infection of psoriasis. It is not unusual to find psoriatic arthritis without previous evidence of psoriasis of the skin or nails.
Symptoms
Symptoms of psoriatic arthritis in the foot include focal swelling of the interphalangeal joint of the toes. The joint will become swollen and painful with no history of injury. X-rays of advanced cases may show slow, erosive changes that are called a pencil and cup deformity. This finding is seen in the metatarsal phalangeal joints where the metatarsal head resembles the point of the pencil and the base of the proximal phalanx (toe) is the receiving cup.
Causes and Contributing Factors
The precise cause of psoriatic arthritis is unknown. Contributing factors include a known history of psoriasis.
Treatment
Treatment of psoriatic arthritis is mostly supportive. Most cases subside within a few months of onset. Severe cases respond to immune therapy similar to the treatment of rheumatoid arthritis.
Reiter's Syndrome
Reiter's Syndrome is an unusual form of arthritis that usually is found in men. Reiter's Syndrome often is described as a sexually transmitted disease because of the disease's history of occurring after sexual intercourse with a partner infected with a chlamydial infection. It is suggested to treat those with Reiter's Disease and their sexual partners for C. trachomatis infections.
Symptoms
The symptoms of RS include burning upon urination (urethritis), dry eyes, and joint pain. Joint pain in the back and feet are common. These symptoms occur 7 to 14 days after intercourse and subside over a period of several months to years. Recurrence of pain is not unusual.
Causes and Contributing Factors
The exact cause of Reiter's Syndrome is unknown. Contributing factors include sexual relations with partners with chlamydial infection.
Treatment
Treatment is often supportive. Symptoms tend to subside in weeks to months.
Differential diagnosis
The differential diagnosis for arthritis of the foot includes:
Bunion
Bursitis
Capsulitis
Cuboid Syndrome
Freiberg's Infraction
Gout
Hallux limitus
Hallus rigidus
Morton's Neuroma
Posterior tibial tendon dysfunction
Pseudogout
Sinus tarsi syndrome
Stress fracture
Tailor's bunion
Tarsal tunnel syndrome
When to Contact Your Doctor
The symptoms of arthritis can vary. Please consult your podiatrist, orthopedist or primary care doctor if you have questions regarding arthritis of the foot and ankle.
Author(s) and date
![]() This article was written by Myfootshop.com medical advisor Jeffrey A. Oster, DPM.
This article was written by Myfootshop.com medical advisor Jeffrey A. Oster, DPM.
Competing Interests - None
Cite this article as - Oster, Jeffrey. Arthritis of the Foot and Ankle. https://www.myfootshop.com/articles/arthritis-of-the-foot-and-ankle
Most recent article update - April 6, 2023.
 Arthritis of the Foot and Ankle by Myfootshop.com is licensed under a Creative Commons Attribution-NonCommercial 3.0 Unported License.
Arthritis of the Foot and Ankle by Myfootshop.com is licensed under a Creative Commons Attribution-NonCommercial 3.0 Unported License.
Internal reference only: ZoneD2, ZoneD3, ZoneD4, ZoneD6, ZoneD7, ZoneL5, ZoneL6, ZoneL8, ZoneM2, ZoneM3, ZoneM4, ZoneM9